Royal Wound Care is the nation’s leading provider of advanced wound care.
Royal Wound Care is a dedicated wound care center located in West Hills, California, specializing in advanced, comprehensive wound treatment. Founded by Dr. Moaddel, Royal Wound Care was born from his commitment to improve the way patients experience wound care. After witnessing the need for more compassionate, personalized care, Dr. Moaddel opened his own center to ensure that every patient receives the attention and expertise they deserve.
After witnessing the shortcomings in traditional wound care settings, Dr. Moaddel set out to create a better experience—one where patients receive the focused, attentive care they truly deserve. That vision became Royal Wound Care.

Our Mission
To deliver exceptional, accessible wound care tailored to the individual—whether in our state of-the-art clinic, at a skilled nursing facility, or in the comfort of a patient’s home. We treat the wound, but we also care for the whole person.
Why Choose Royal Wound Care?
Ongoing Education & Certification
For staff, families, and partner facilities, including wound in-services and professional training opportunities
Expert-Led Care by Board-Certified Providers
With years of hands-on experience managing chronic and complex wounds
Advanced Modalities
Including negative pressure therapy, mist ultrasound, debridement, Doppler studies, grafts, and more
Survey-Ready Documentation
That keeps facilities compliant and families informed
Truly Personalized Care Plans
Tailored to each patient’s condition, lifestyle, and healing goals
Mobile Services That Come to You
Care delivered at home, in clinics, or within partner facilities
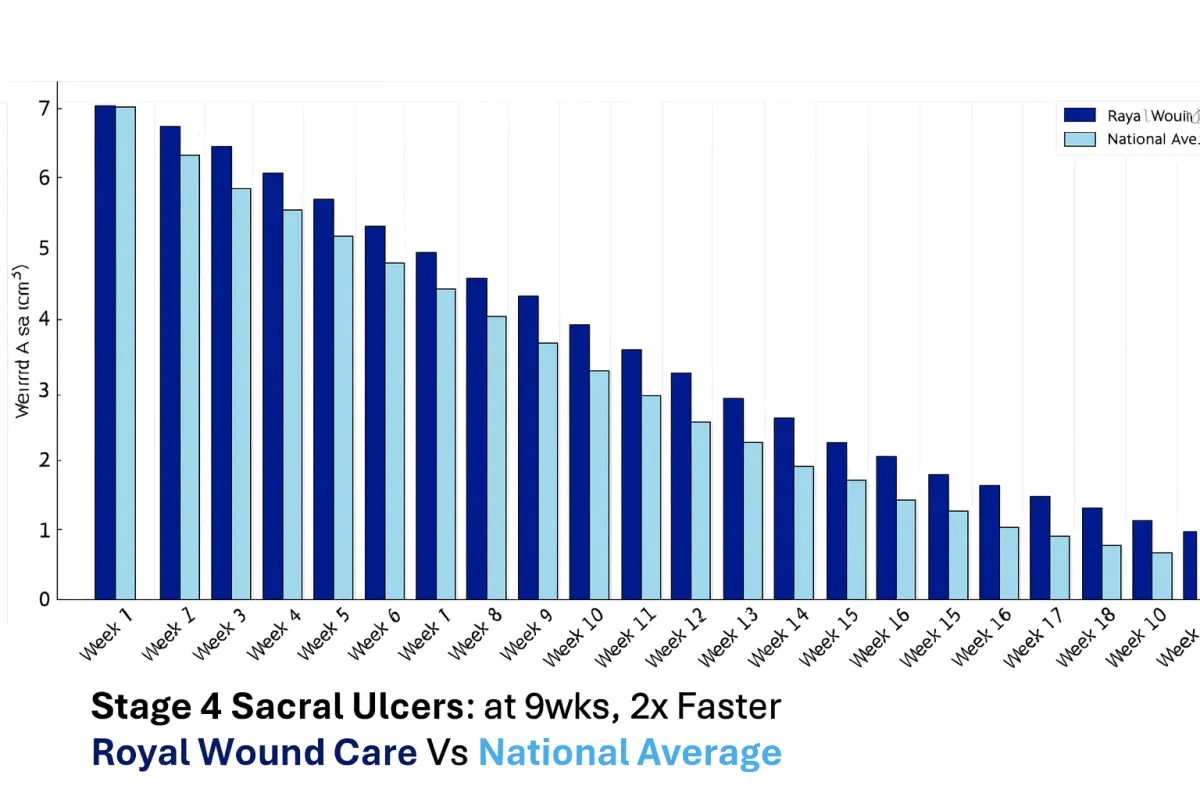
A Team That Cares And The Results To Prove It
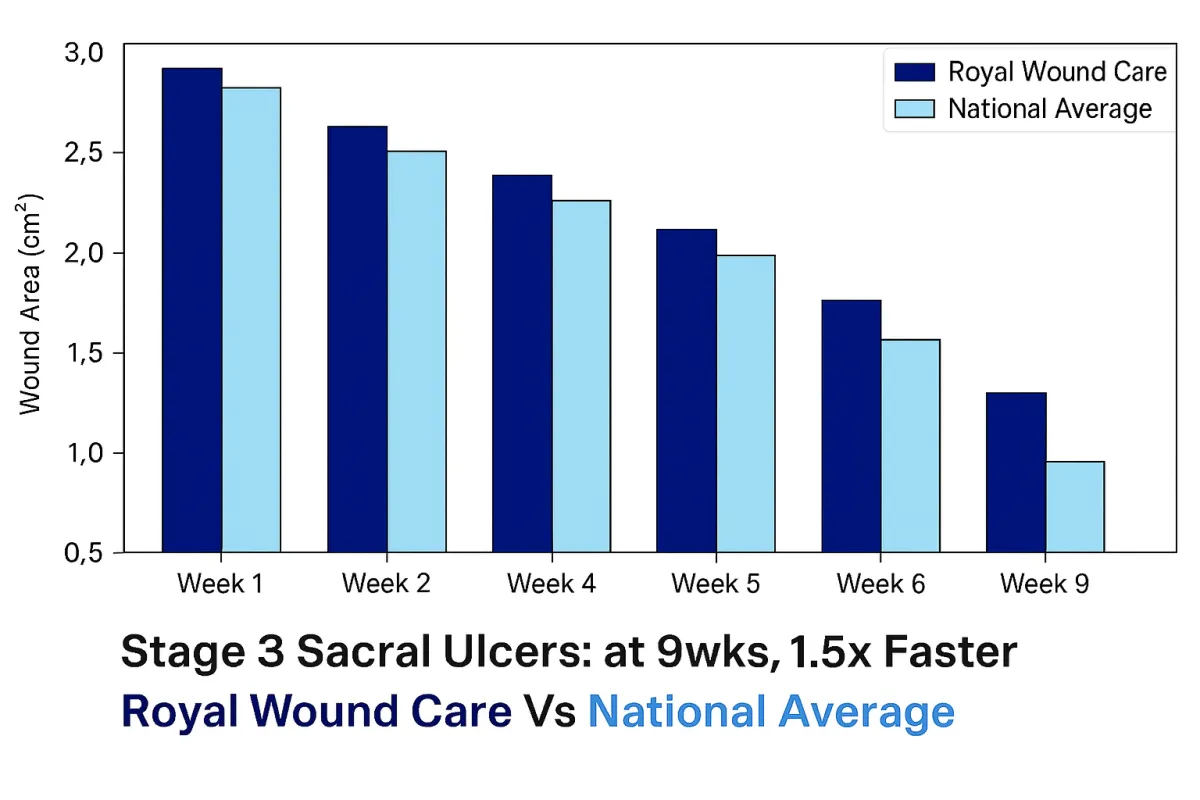
At Royal Wound Care, we deliver results that consistently outperform the national average. Our advanced healing process combines evidence-based treatments, personalized care plans, and direct physician oversight to ensure optimal outcomes. Unlike many clinics, every patient is managed by a board-certified wound care physician who evaluates their condition and customizes treatment from day one.
Our Stage 3 Sacral ulcer graph demonstrates how our approach leads to significantly faster healing compared to the national average. While traditional care results in gradual wound size reduction over several months, patients treated at Royal Wound Care experience more rapid progress through targeted therapies, aggressive infection control, and ongoing physician-directed adjustments to their care plan. Our proactive methods allow us to close even complex wounds weeks earlier than national trends, improving patient mobility, reducing pain, and preventing further complications.
Stage 4 sacral ulcers are among the most complex wounds to treat, yet our outcomes set us apart. Patients at Royal Wound Care heal twice as fast as the national average by leveraging advanced biologic grafts, comprehensive infection management, and customized care protocols. These results highlight our proactive, physician-led care model, allowing us to manage even the most challenging cases successfully while improving long-term patient outcomes.
What Our Partners Experience
86% lower infection rates
47% faster healing compared to others
88% fewer wound-related rehospitalizations
58% faster pressure ulcer healing times
Ready to Heal with Royal Wound Care?

Wound Care for Diabetic Foot Ulcers: Causes and Treatment
Wound Care for Diabetic Foot Ulcers: Causes and Treatment
When discussing diabetes, the role the condition plays in wound healing often goes overlooked. High blood sugar can damage nerves, impair circulation, weaken the immune system, and result in both slow-healing and chronic wounds. More specifically, diabetic foot ulcers (DFUs) are extremely prevalent—affecting an estimated 18.6 million people worldwide.
These injuries are more than skin deep. With how quickly they can progress, diabetic wounds often require specialized wound care and advanced treatments to avoid lifelong discomfort. Nonetheless, proper education makes all the difference in both prevention and treatment.
With this in mind, this patient-led guide focuses on risk factors, prevention strategies, and optimal care plans for diabetic foot ulcers. With expert insights and evidence-based approaches, patients can heal faster, safer, and more effectively.
Best Wound Care for Diabetic Foot Ulcers: Effective Treatment Options
Recent research shows that over the span of their lifetime, people with diabetes face a 19% to 34% risk of developing a DFU. However, at Royal Wound Care, we take pride in advanced personalized care plans, expert-led care, and improved patient outcomes. It all begins with awareness and education.
Below, we will start by discussing what a diabetic foot ulcer is. Afterwards, we’ll explain the causes of DFUs, the risk factors that play a role in delayed wound healing, and the proper treatment methods that support successful recovery.
For many patients, diabetic foot ulcers can feel intimidating to manage. However, know that 60-80% of DFUs do heal with effective support.
Related: How Can a Diabetic Wound Heal Faster?
What Is a Diabetic Foot Ulcer?
A diabetic foot ulcer is an open sore or wound that appears on the feet of someone with diabetes. Most commonly, these injuries occur on the bottom of the foot or on pressure points around the heels and toes. The wounds begin as minor injuries that slowly progress, breaking down tissue and exposing underlying layers.
Foot ulcers in patients with diabetes are more common due to a combination of factors—many of which we will discuss below. However, for most, nerve damage (neuropathy) reduces feeling, leading to a loss of sensation and unnoticed injuries.
What generally begins as a small cut or blister from walking barefoot or wearing tight shoes can, without detection, rapidly progress. With an increased risk of infection due to a compromised immune system, high-quality wound care becomes pivotal in recovery.
Related: Diabetic Wound Care: Specialized Treatment for Optimal Healing
What Causes Diabetic Foot Ulcers?
High Blood Glucose Levels
High blood glucose levels, also commonly known as high blood sugar, are the root cause of many diabetic foot ulcers. Most commonly, this factor plays a significant role in nerve damage—which we will discuss below. However, there are several additional ways high blood sugar contributes to diabetic wound development.
To start, elevated glucose levels can slow immune response—specifically, the function of white blood cells. Because these cells are the body’s main defense against bacteria, the risk of infection increases. This is how even minor abrasions can quickly develop into serious injuries—even if a patient isn’t experiencing a loss of sensation.
Consider high blood sugar as one of the root causes of the factors we will discuss below.
Reduced Circulation and Peripheral Artery Disease
Through a combination of high blood sugar and chronic inflammation, diabetes can damage both small and large blood vessels. As these vessels narrow and harden, it’s extremely common to experience reduced circulation.
In many cases, this reduced blood flow is linked to Peripheral Artery Disease (PAD), a condition where major arteries in the extremities become blocked. As a result, the tissue in the legs and feet doesn’t receive the oxygen and nutrients necessary for healing ulcers.
According to data, PAD is 9-55% more common in those with diabetes. However, it’s essential to note that not all diabetics who experience reduced circulation have PAD—and vice versa. Microvascular circulation is also common but far more subtle.
Related: Edema and Diabetes and Slow Healing Wounds: Understanding Care
Nerve Damage (Peripheral Neuropathy)
The longer nerves go without oxygen and nutrients, the more likely they are to become damaged—a condition known as peripheral neuropathy. Because of this, patients may become unable to feel pain, temperature changes, or sustained pressure.
This is why many minor cuts and blisters commonly go unnoticed. Combined with impaired skin integrity, the feet can become chronically dry, cracked, and prone to injury. With repetitive pressure or unintentional disregard, injuries worsen before proper wound care begins.
If left untreated, peripheral neuropathy can result in life-threatening infections, amputations, and heart disease. However, by using a strategic care plan, wound care specialists can successfully manage and even reverse this condition.
Related: Caring for Your Wound
Reduced Growth Factors
Diabetes impairs the body’s ability to produce growth factors responsible for cell repair. More specifically, chronic high blood sugar disrupts cell proliferation and regeneration, two processes essential for tissue growth.
Additionally, diabetes can impair angiogenesis—the formation of new blood vessels. Reduced growth factors (GFs) ultimately compromise the body’s ability to advance through the normal stages of wound healing. This makes healing ulcers more challenging, increasing the likelihood of slow-healing or chronic wounds.
Additional Lifestyle Factors
Lifestyle factors, comorbidities, and prior health history all play significant roles in wound healing. These may include:
Immune dysfunction
Smoking
Reduced physical activity
Diabetes-related complications
Nutritional status
Wound duration
Alcohol consumption
Obesity
Ultimately, it’s essential to understand how underlying conditions can impact wound healing and treatment success. When a patient successfully manages or addresses additional influences, they can directly shape the healing process and reduce the risk of complications.
Related: Nutrition and Wound Healing: What to Eat for Faster Wound Healing
How To Care For a Diabetic Foot Ulcer
Caring for a diabetic foot ulcer requires more than standard first-aid. Proper wound care involves medical evaluation, infection prevention, ongoing monitoring, and personalized treatment plans.
If you or a loved one is managing a DFU, these expert-backed tips can aid in recovery, treatment, and overall comfort:
Keep the Wound Clean and Dressed
The first and often most important step in proper wound care is keeping the ulcer clean and bandaged.
To start, cleanse the ulcer to remove debris, bacteria, and dead tissue. If left unattended, these can influence and interfere with the healing process. Ensure you avoid harsh antiseptic treatments, such as hydrogen peroxide or alcohol, to avoid drying out the wound. It’s crucial to keep the wound moist.
Instead, antimicrobial ointments, hydrating gels, or prescribed topical treatments can all create an optimal healing environment. After cleansing, use wound dressings to protect the injured area. Similar to the cleanser, the type of dressing can significantly influence healing. Opt for a moisture-retentive, antimicrobial, or collagen-infused dressing.
Related: How Long Does It Take for a Wound to Heal: What Every Nurse and Patient Should Know
Manage Blood Glucose Levels
Blood sugar levels influence every stage of the healing process—especially in cases of diabetic foot ulcers. If a patient consistently has high levels, this can continue to compromise immune function and damage blood vessels.
As a result, it becomes significantly more challenging to address and heal a DFU. Working with a provider to maintain stable glucose levels encourages a quicker, healthier immune response. This can positively impact cell migration, white blood cell function, oxygen and nutrient flow, and tissue regeneration.
Reduce Pressure on the Foot
As previously discussed, for patients dealing with decreased sensations, it becomes difficult to feel both pain and pressure. If left unmonitored, any additional pressure can further restrict blood flow and irritate injured tissue.
Relieving any unnecessary pressure is essential to prevent new injuries from forming or current injuries from worsening. This can be as easy as removing shoes, braces, or custom inserts. With this, patients with reduced circulation should use warm compresses and practice foot elevations to encourage better blood flow.
Related: Pressure Ulcers and Wound Care
Monitor for Infections
Individuals with diabetes face a higher risk of infection due to impaired immune function, poor circulation, and potential nerve damage. Because of this, it’s vital to continue monitoring for any infection.
The sooner a patient is able to recognize the signs, the quicker they can intervene to reduce complications. Signs of a diabetic foot ulcer infection may include: swelling, odor, drainage, increased pain, warmth, or fever.
Related: Signs It’s Time to Get Expert Help
Seek Assistance from a Specialized Wound Care Clinic
For patients with diabetes, professional assistance from a specialized clinic can make a drastic difference in healing. At Royal Wound Care, we pride ourselves on exceptional, accessible care tailored to each unique individual. While diabetes impacts an estimated 38 million Americans, every person, every wound, and every situation is different.
We offer cutting-edge therapies, such as UltraMist® Therapy, Wound VAC Therapy, skin substitutes, biological dressings, and hyperbaric oxygen therapy. Additionally, routine appointments allow our providers to assess the healing process, adjust dressings, discuss risk factors, and provide treatment that reduces future complications.
As challenging as diabetic foot ulcers can be, the right support can lead to faster, more effective healing.
With the right knowledge and consistent care, diabetic foot ulcers can be managed effectively to support long-term health outcomes.
Diabetic foot ulcers are a common and serious complication for individuals living with diabetes. However, they don’t behave like general wounds. Between blood glucose levels, reduced circulation, and nerve damage, healing requires consistent care and medical support. By understanding contributing factors, patients can take proactive steps toward safer healing and prevention.
At Royal Wound Care, we understand the role proper care plays in long-term comfort and overall quality of life. Through mobile wound care, in-clinic wound care, and home health care, we meet patients exactly where they are in their healing journey. Contact us today to learn more about how we can help heal diabetic foot ulcers.
For SNFs or independent nurses, we offer advanced education opportunities and professional partnerships to lower facility costs, infection rates, and reduce re-hospitalizations. Let’s bridge the gap between accessibility and quality care—together.
WEST HILLS
7230 Medical Center Dr. Suite 100
West Hills, CA 91307
(818)–660–2977
BEVERLY HILLS
9735 Wilshare Blvd #210B
Beverly Hills, CA 90212
(818)–660–2977
If you are interested in making an appointment, please click here to find a Wound Care Center near you.
Request an Appointment at a Royal Wound Care Facility near you.
Royal Wound Care is the expert in wound healing. Our board-certified wound care specialists are ready to help you begin your healing journey. Click the button below to request an appointment at a Wound Care Center near you—no referral needed
© 2025 Royal Wound Care, LLC. All rights reserved.
site by Growth Partners Marketing