Royal Wound Care is the nation’s leading provider of advanced wound care.
Royal Wound Care is a dedicated wound care center located in West Hills, California, specializing in advanced, comprehensive wound treatment. Founded by Dr. Moaddel, Royal Wound Care was born from his commitment to improve the way patients experience wound care. After witnessing the need for more compassionate, personalized care, Dr. Moaddel opened his own center to ensure that every patient receives the attention and expertise they deserve.
After witnessing the shortcomings in traditional wound care settings, Dr. Moaddel set out to create a better experience—one where patients receive the focused, attentive care they truly deserve. That vision became Royal Wound Care.

Our Mission
To deliver exceptional, accessible wound care tailored to the individual—whether in our state of-the-art clinic, at a skilled nursing facility, or in the comfort of a patient’s home. We treat the wound, but we also care for the whole person.
Why Choose Royal Wound Care?
Ongoing Education & Certification
For staff, families, and partner facilities, including wound in-services and professional training opportunities
Expert-Led Care by Board-Certified Providers
With years of hands-on experience managing chronic and complex wounds
Advanced Modalities
Including negative pressure therapy, mist ultrasound, debridement, Doppler studies, grafts, and more
Survey-Ready Documentation
That keeps facilities compliant and families informed
Truly Personalized Care Plans
Tailored to each patient’s condition, lifestyle, and healing goals
Mobile Services That Come to You
Care delivered at home, in clinics, or within partner facilities
A Team That Cares And The Results To Prove It
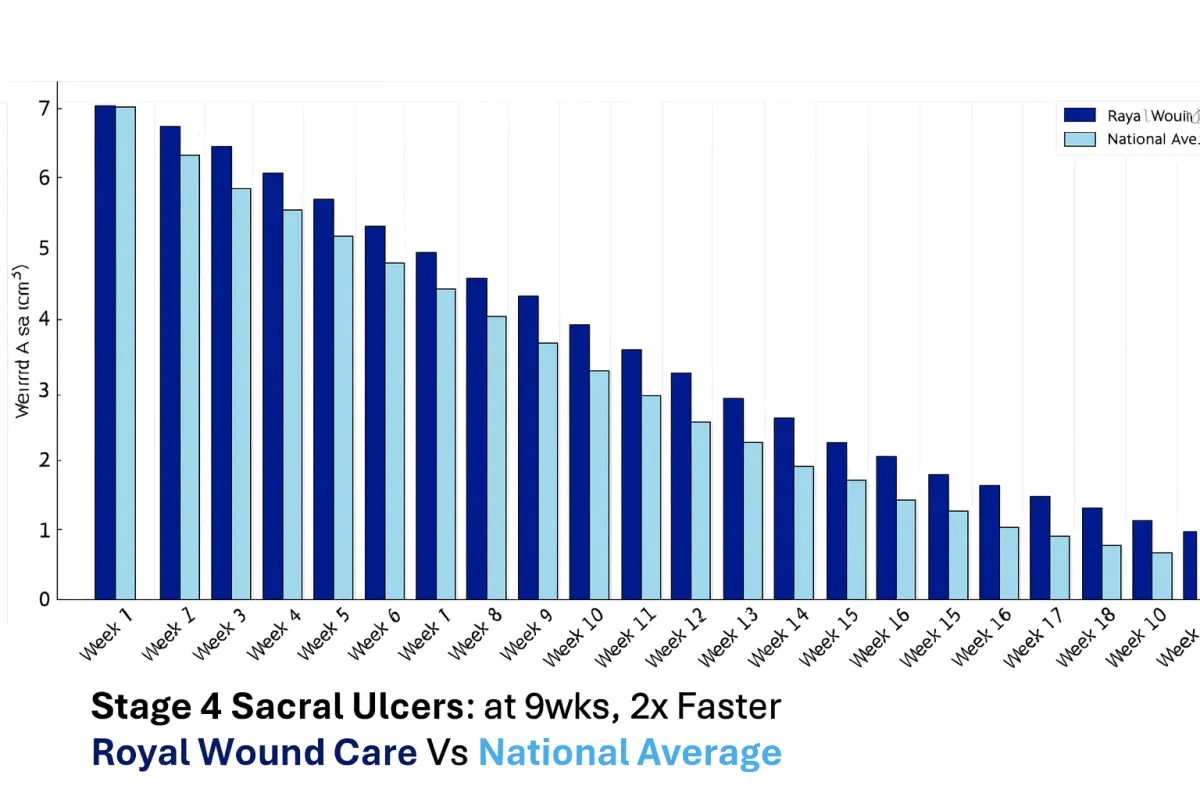
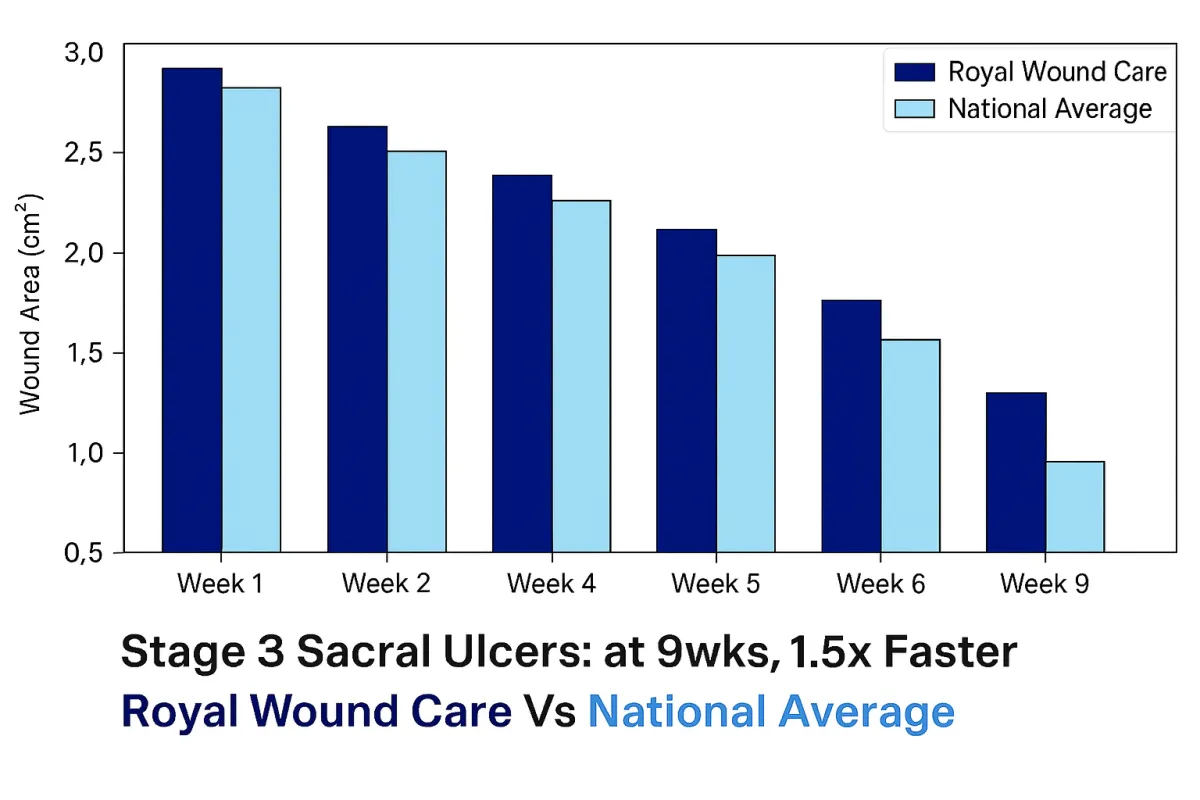
At Royal Wound Care, we deliver results that consistently outperform the national average. Our advanced healing process combines evidence-based treatments, personalized care plans, and direct physician oversight to ensure optimal outcomes. Unlike many clinics, every patient is managed by a board-certified wound care physician who evaluates their condition and customizes treatment from day one.
Our Stage 3 Sacral ulcer graph demonstrates how our approach leads to significantly faster healing compared to the national average. While traditional care results in gradual wound size reduction over several months, patients treated at Royal Wound Care experience more rapid progress through targeted therapies, aggressive infection control, and ongoing physician-directed adjustments to their care plan. Our proactive methods allow us to close even complex wounds weeks earlier than national trends, improving patient mobility, reducing pain, and preventing further complications.
Stage 4 sacral ulcers are among the most complex wounds to treat, yet our outcomes set us apart. Patients at Royal Wound Care heal twice as fast as the national average by leveraging advanced biologic grafts, comprehensive infection management, and customized care protocols. These results highlight our proactive, physician-led care model, allowing us to manage even the most challenging cases successfully while improving long-term patient outcomes.
What Our Partners Experience
86% lower infection rates
47% faster healing compared to others
88% fewer wound-related rehospitalizations
58% faster pressure ulcer healing times
Ready to Heal with Royal Wound Care?

Diabetic Wounds on Legs: Why They Form and How to Treat Them
Diabetic Wounds on Legs: Why They Form and How to Treat Them
Wound care is an intricate process—one that is significantly affected by underlying conditions, such as diabetes. This condition impacts nearly every system in the body, including the skin, nerves, and blood vessels. However, while an estimated 38 million Americans live with diabetes, many are unaware of how it impacts wound healing.
As we discussed previously, diabetic foot ulcers are among the most frequently treated complications in wound management. However, while less common, leg ulcers are equally challenging. Poor circulation and reduced blood flow can delay healing and contribute to chronic wound development, increasing the risk of life-threatening complications.
At Royal Wound Care, we believe treatment begins with proper education. To help, today’s post serves as a comprehensive, patient-focused guide to diabetic wounds on legs. We will discuss how diabetes impacts wounds, what leg sores look like, and how to effectively treat them. Expert insights are the first step to safer, more efficient healing.

Diabetic Wounds on Legs: Why They Form and How to Treat Them
Many patients often assume that uncontrolled blood sugar is the leading cause of non-healing open wounds. However, this isn’t always the case. While managed sugar can significantly reduce risk, it doesn’t eliminate it completely.
From high blood pressure and poor circulation to nerve damage and a weakened immune system, there are many reasons why people with diabetes experience both foot and leg ulcers. And today, we’re here to discuss it.
Whether you’re facing a leg ulcer for the first time or dealing with a chronic ulcer that keeps returning, proper care is essential to quality of life and long-term healing.
Related: Managing Chronic Wounds: A Comprehensive Guide
Does Diabetes Cause Sores on Legs?
Yes, diabetes can cause sores on legs. In fact, studies show that people with diabetes have a 15-25% chance of developing an ulcer at some point. Additionally, research states that ulcers above the malleoli (the bumps on the inner and outer sides of the ankle) are almost as common as foot ulcers.
Ultimately, ulcers develop due to a combination of symptoms. Some of these include diabetic neuropathy (nerve damage), reduced blood flow from peripheral arterial disease (PAD), and narrowed vessels. At the heart of it all, however, lie high blood sugar levels.
High blood sugar can damage nerves and weaken the blood vessels that supply the legs. As a result, patients begin to experience a lack of sensation in the lower extremities. As opposed to feeling a minor scrape or consistent pressure, diabetics may not notice or realize skin irritation until the wound has progressed.
Additionally, elevated glucose levels can slow the immune response. A combination of impaired white blood cell function and reduced oxygen and nutrient delivery to the affected area makes it even more difficult for the body to recover and for wounds to heal.
Without proper care, these wounds can lead to amputation, severe infections, worsening pain, and tissue death. Most importantly, however, they can significantly decrease a patient’s quality of life. Following expert-led advice is essential for helping wounds heal faster, safer, and more effectively.
Related: Diabetic Wound Care: Specialized Treatment for Optimal Healing

What Do Diabetic Leg Sores Look Like?
Diabetic leg sores can appear differently based on several factors, including severity, circulation, and infection risk. However, here are general guidelines to look for based on the University of Texas (UT) Classification wound stages:
Grades (Wound Depth):
Grade 0: Ulcerative site that has completely healed
Grade 1: Superficial wound that does not involve exposure of the tendon, joint capsule, or bone
Grade 2: Wound that has penetrated beyond superficial layers; is reaching tendon or joint capsule, but not yet bone
Grade 3: A deep diabetic ulcer that has fully penetrated the bone or joint
Classification Stages:
Stage A: Pre-ulcerative lesions; there is no skin break, no restriction of blood supply, and no infection
Stage B: Infected wounds that still have adequate blood flow
Stage C: Slow-healing wounds with lack of blood flow; doesn’t show signs of infection, but are more prone to it
Stage D: Wounds with both a lack of blood flow and a current infection
What to look for:
Redness, discoloration, or shiny patches of skin
Dry, fragile skin that cracks easily
Areas that are warm, swollen, or tender
A small open wound that slowly grows larger
Yellow, white, or brown tissue inside the ulcer
Drainage, older, or increasing pain
Increased firmness (callus) surrounding the wound
Wounds caused by peripheral artery disease (PAD) often look “punched out.” They will have well-defined edges, appear discolored, and can sometimes ooze or bleed. Early identification makes all the difference in how a wound heals.
Additionally, although commonly confused, the appearance of diabetic leg ulcers is significantly different from that of venous ulcers. To learn more, visit: “How to Treat Venous Ulcers and Leg Swelling Effectively.”

How to Treat Diabetic Leg Wounds
Maintain Blood Sugar Levels
In terms of healing diabetic leg ulcers, maintaining blood sugar levels is the first and most crucial step. When doing so, patients can experience improved circulation, stronger immunity, enhanced cell function, and increased levels of growth factors.
As a result, cells can successfully repair and build new tissue, encouraging the wound to heal and close faster. Additionally, growth factors support the body’s natural healing signals, such as epithelial cells, connective tissue, blood vessels, and white blood cells. When these systems work together, the body is more equipped to prevent complications and heal successfully.
Related: How Long Does It Take for a Wound to Heal: What Every Nurse and Patient Should Know
Clean and Dress the Wound Properly
Whether patients opt for self-care, home health care, or in-clinic wound care, cleaning and dressing wounds is essential for healing. To start, cleaning the ulcer effectively removes pathogens, debris, bacteria, and dead tissue.
However, it’s important to avoid harsh antiseptics—like hydrogen peroxide or alcohol—and instead use antimicrobial ointments, hydrating gels, or prescribed topical treatments.
Moreover, wound dressings further protect the injured area from harmful external factors. Just like with cleansers, the type of dressing can significantly influence the healing timeline. Opt for moisture-retentive, antimicrobial, or collagen-infused dressings.
Related: Caring for Your Wound
Don’t Ignore Infection Warning Signs
As we discussed before, many individuals with diabetes experience reduced sensation. Because of this, even if they’re aware of a wound, they may not be able to feel pain, pressure, or worsening symptoms that signal the injury is becoming more severe.
To catch things before they progress, it’s essential to continue monitoring the area for any warning signs. This includes redness, increased warmth, swelling, pus or drainage, a foul odor, increased pain, firmness, or non-healing wounds. If caught early, patients can visit a specialist before severe complications arise.
Implement Diet and Lifestyle Changes
When managing diabetic wounds, every seemingly minor thing matters. Lifestyle factors, health history, and comorbidities can delay healing or lead to chronic ulcers. To start, we recommend re-evaluating lifestyle changes where possible.
For example, high blood pressure, smoking, and consuming alcohol can impair immune response, increase infection risk, and hinder healing. When addressed and managed early, patients can actively work with physicians to improve the body’s ability to heal.
Additionally, nutrition and diet have a key role in healing timelines. Wound healing is complex, and the proper vitamins, minerals, and nutrients can provide the body with fuel it needs to heal.
Related: Nutrition and Wound Healing: What to Eat for Faster Wound Healing
Know When to Visit a Wound Care Specialist
When managing diabetes, both leg and foot care can often feel challenging and isolating. However, reaching out to specialized wound care specialists can make a significant difference throughout the process.
At Royal Wound Care, we pride ourselves on accessible, exceptional care tailored to each individual. We don’t just aim to treat the wound—we care for each person as a whole. Along with expert-led advice and unique care plans, we also offer advanced wound treatments that accelerate healing and improve lives.
From debridement and UltraMIST® Therapy to wound VAC therapy and skin substitutes, healing isn’t only possible—it’s within reach.
Related: When to See a Wound Care Specialist: Signs It’s Time to Get Expert Help
With intentional lifestyle changes and wound care specialists, diabetic wounds on legs don’t have to determine long-term health outcomes.
It’s not uncommon for individuals with diabetes to experience foot ulcers, leg ulcers, and non-healing wounds. However, commonality doesn’t make them any less challenging. With the right approach, intentional lifestyle changes, and intervention from a specialized wound care clinic, healing is just around the corner.
At Royal Wound Care, we understand the importance of bridging the gap between accessibility and recovery. This is why we offer in-clinic services and mobile wound care. Patients don’t have to live with chronic pain or risky complications. We’re here to heal, help, and protect you—no matter what your wound looks like.
Additionally, we offer advanced education opportunities and professional partnerships for both SNFs and independent nurses. With reduced re-hospitalizations, lower infection rates, and improved patient outcomes, healing has never felt more promising.
WEST HILLS
7230 Medical Center Dr. Suite 100
West Hills, CA 91307
(818)–660–2977
BEVERLY HILLS
9735 Wilshare Blvd #210B
Beverly Hills, CA 90212
(818)–660–2977
If you are interested in making an appointment, please click here to find a Wound Care Center near you.
Request an Appointment at a Royal Wound Care Facility near you.
Royal Wound Care is the expert in wound healing. Our board-certified wound care specialists are ready to help you begin your healing journey. Click the button below to request an appointment at a Wound Care Center near you—no referral needed
© 2025 Royal Wound Care, LLC. All rights reserved.
site by Growth Partners Marketing