When Should Sutures Be Removed? Types, Timing, and Care
When Should Sutures Be Removed? Types, Timing, and Care
Sutures play many critical roles in the wound healing process. On the surface, they physically bring separated tissue together, encouraging accelerated healing and scar minimization. However, there’s far more to tissue regeneration than surface-level wound closure.
Sutures close an open wound layer by layer, beginning at the deepest tissues (muscle fascia), working up to the outer layer of the skin. In doing so, they provide tension relief, structural support, and infection prevention, all of which are necessary for optimal healing. However, knowing when sutures should be removed is just as important as proper placement.
Improper removal can result in wound dehiscence (reopening), delaying healing and increasing the risk of complications. For patients, understanding the proper timeline is essential for setting expectations and supporting care habits. Therefore, in this guide, we will discuss how different sutures work and how timing plays a key role in safe healing.

When Should Sutures Be Removed? Types, Timing, and Care
At Royal Wound Care, we believe that expert-led education is one of the most important steps in effective healing. Additionally, managing wounds is often a complex journey—especially when patients feel they’re navigating unexpected timelines.
To encourage proper care, we’re exploring a clear, clinician-guided timeline for suture removal. We’ll discuss what sutures are, how different materials can impact removal timelines, and what to expect during the process. We’ll also explain why following physician care instructions is essential for reducing complications and supporting long-term healing.
Remember: these small tools, while uncomfortable at times, make all the difference in overall recovery. This guide is designed to reassure, answer common questions, and support confident decisions.
Related: How Long Does It Take for a Wound to Heal? What Every Nurse and Patient Should Know
What Are Sutures?
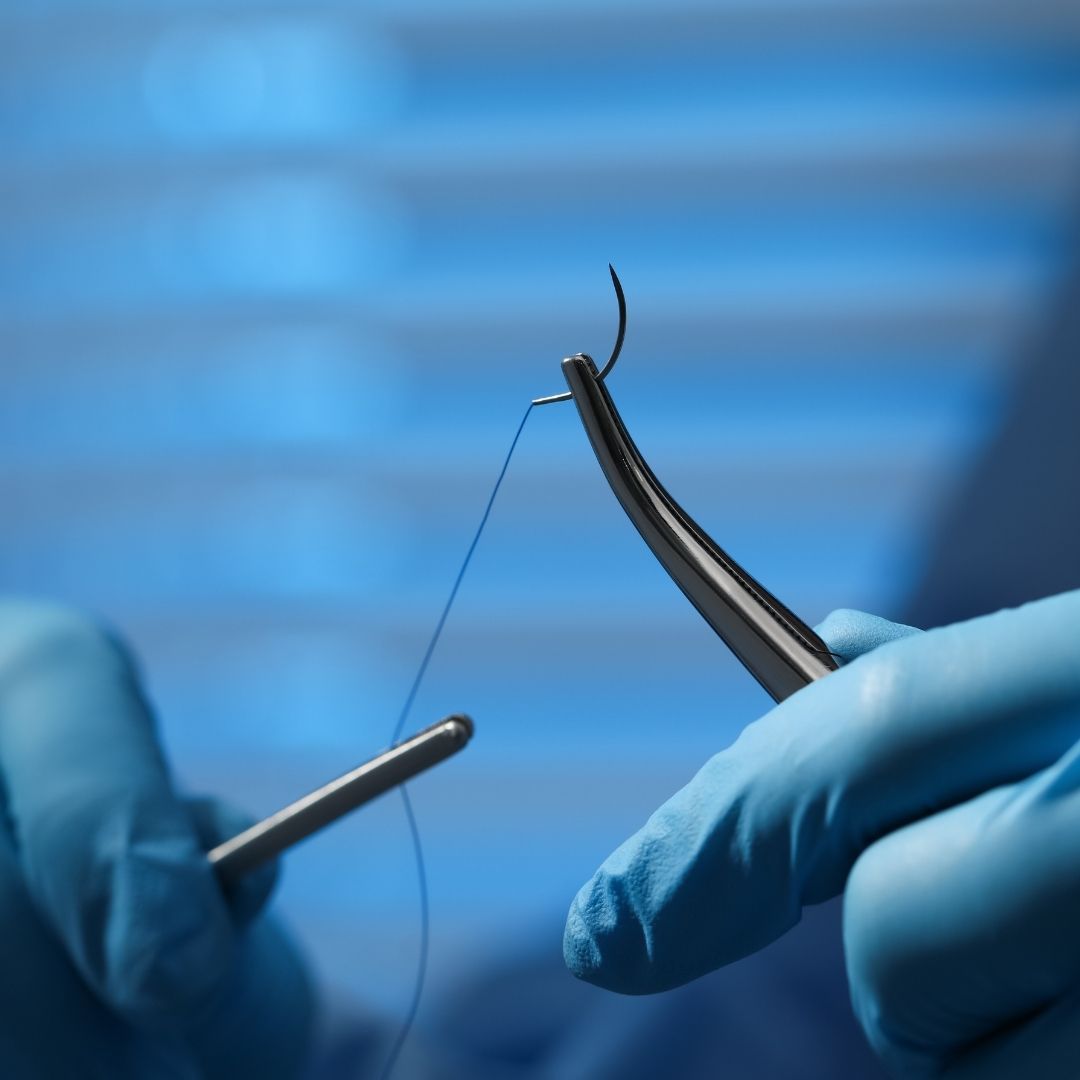
Sutures, also commonly referred to as stitches, are sterile medical threads used to sew wounds and surgical incisions together. Their primary purpose is to hold tissue in place as the body repairs itself over a specific period.
By keeping the wound closed and the edges aligned, sutures simultaneously reduce bleeding, minimize the risk of infection, and support proper closure. Ultimately, however, a lot is going on underneath the surface.
Sutures provide a scaffold for epithelial cells to close the surface barrier and regenerate the skin surface—also known as re-epithelialization. Simultaneously, fibroblasts build new connective tissue and support collagen synthesis, strengthening the wound bed and restoring structural integrity.
Depending on the wound, sutures can be applied both on the surface and deeper into the tissue layers. Because of this, they are often combined with other effective wound care techniques. Examples include advanced dressings, growth factors, antibiotic ointment, and continuous monitoring.

What Are the Different Types of Sutures?
Absorbable Sutures
Absorbable sutures (also referred to as dissolvable stitches) break down in the body over time. Generally, this type of suture is used for deeper layers of tissue, such as muscle layers or internal organs—areas where removal is either too difficult or unnecessary.
However, the absorption process is entirely safe, as the body naturally flushes out the smaller components over time. As a result, patients do not have to visit a clinic for official removal, ultimately simplifying recovery and reducing discomfort. However, it’s essential to follow your physician’s instructions and monitor for signs of infection or irritation.
Related: Caring for Your Wound
Temporary Non-Absorbable Sutures
Non-absorbable sutures are surgical threads that the body does not naturally break down. Instead, they remain in place until a patient visits a physician to physically have their stitches removed. However, the process is generally straightforward, causing minimal tissue reaction and faster healing.
In most cases, a doctor will apply temporary non-absorbable sutures to either external skin or wounds in high-tension, slow-healing areas. This type of suture is also often used in cosmetic surgeries where controlled removal minimizes scarring. Ultimately, a physician or a wound care specialist can determine the unique timeline of removal.
Permanent Non-Absorbable Sutures
Permanent non-absorbable sutures are sutures that do not dissolve in the body and are designed to provide long-term wound support. More specifically, doctors apply them to slow-healing tissues and high-tension areas.
Examples include cardiovascular surgeries, orthopedic procedures, hernia repair, and neurosurgical implants. Essentially, they make up the tensile strength that the body cannot provide on its own. They also provide reinforcement to the injury, making sure the area remains stable indefinitely.

How Are Sutures Classified?
Sutures are grouped based on how they’re made and what they’re made from. To clarify, the first two classifications focus on structure, while the remaining categories describe the material type.
Monofilament Sutures
Monofilament sutures are a specific surgical thread that is made from a single strand of material. Additionally, monofilament sutures can be both absorbable and non-absorbable, depending on the wound type and severity.
They’re known for their smooth design, reducing tissue drag and the likelihood of harboring bacteria. This structure is ideal for both delicate areas and infected wounds, as it causes less additional inflammation and trauma. In many cases, physicians use monofilament sutures for blood vessel repair, vascular surgery, and cosmetic closure.
Multifilament Sutures
Multifilament sutures consist of multiple surgical threads braided together. In comparison to monofilament sutures, they offer better knot security, easier handling, and higher tensile strength. As mentioned previously, however, this structure can be both absorbable and non-absorbable.
Because of their versatility, doctors commonly use multifilament sutures for deep tissue closure, cardiac procedures, and intestinal anastomoses. That said, they’re also more likely to harbor bacteria, making careful monitoring essential.
Natural Sutures
Natural sutures are biodegradable surgical threads that the body can safely absorb or break down. Additionally, natural sutures are made primarily from silk, cotton, linen, or catgut (a collagen-based material).
However, contrary to its name, this material may provoke a stronger reaction from some patients due to the inflammatory process required for absorption. Because natural sutures require enzymatic digestion, common side effects may include inflammation, granulomas, and allergic reactions.
Synthetic Sutures
Synthetic sutures are surgical threads made from man-made polymers. Non-absorbable sutures typically use materials like polyester (Mersilene), Polypropylene (Prolene), and Nylon (Ethilon).
In comparison, absorbable synthetic sutures use materials such as Polyglactin 910 (Vicryl), Polyglycolic Acid (Dexon), and Polydioxanone (PDS). Given that they break down by hydrolysis, synthetic sutures are the preferred choice by physicians for patient safety, healing, and comfort.
Do Sutures Need to Be Removed?
Not all sutures require removal. As mentioned earlier, absorbable sutures naturally dissolve, while permanent non-absorbable sutures provide long-term relief. However, a healthcare professional must remove temporary non-absorbable sutures once healing is complete.
Nonetheless, even if a patient’s sutures do not require removal, ongoing care is just as essential. This involves keeping the area clean, applying antibiotic ointment as directed, and monitoring for any signs of infection. It’s crucial that a patient does not attempt to remove sutures by themselves or by an unqualified participant.
Doing so may reopen the wound, lead to improper healing, increase the risk of infections, or worsen scarring. Most importantly, premature removal can result in a chronic, non-healing wound—a serious and potentially life-threatening complication.
Related: Effective Chronic Wound Care Strategies
When to Remove Sutures
The timeline for suture removal depends on the wound site and the body’s response. Below are general guidelines for healing. However, individual recommendations may vary. To learn more, visit: “When to See a Wound Care Specialist: Signs It's Time to Get Expert Help.”
Face
Average Removal Timeline: 3–7 days (as early as 48 hours for select wounds)
For superficial face wounds, many physicians remove fast-absorbing sutures as early as 48 hours. However, the standard timeline ranges from 3 to 7 days. Eyelids and lips, for example, don’t require nearly as much time to heal due to a strong blood supply. In comparison, the chin and the ears may require longer due to greater movement and less soft-tissue coverage.
Scalp
Average Removal Timeline: 7–10 days
The scalp is another area of the body that heals relatively quickly. While slower healing than the face, rich blood supply and hair follicle stem cells contribute significantly to re-epithelialization. Ultimately, hair thickness can also impact healing, so the general timeline varies.
Arms and Hands
Average Removal Timeline: 7–14 days
Where an injury occurs on both the hands and arms can significantly impact suture removal timelines. Wounds on the arms often require closer to the 10-14 day mark due to increased movement, greater tension, and deeper tissue involvement. In comparison, the hands and fingers heal surprisingly fast due to increased blood supply and specialized cells.
Joints
Average Removal Timeline: 10–14+ days
Because the joints experience consistent movement and mechanical stress, the skin edges often take longer to bond. Otherwise, the wounds will continue to stretch and reopen. And, generally speaking, tissues in both extremities and joints take longer to heal due to a complex blood supply.
Legs and Feet
Average Removal Timeline: 10–14 days
Lower-extremity wounds heal more slowly due to reduced circulation, making it harder for oxygen and nutrients to reach the wound bed. In addition to this, gravity pulls fluid downwards, increasing swelling and straining at the injury site. In most cases, doctors can safely remove sutures after 10-14 days. However, individual cases and timelines vary.
Related: Edema and Diabetes and Slow Healing Wounds: Understanding Care
When managed with proper timing and professional care, suture removal becomes a safe, effective step in wound healing.
There are many reasons a patient might need sutures—from surgical incisions to minor scalp abrasions. However, knowing when they should be removed empowers individuals to take an active role in their recovery. With proper timing and attentive care, sutures are essential for safe wound closure and long-term healing.
At Royal Wound Care, we pride ourselves on expert, compassionate wound care services. From initial diagnosis to wound recovery, our team combines cutting-edge research with a highly trained, board-certified staff to reduce complications and improve outcomes.
When navigating wound management with Royal Wound Care, you’re never alone. For questions or concerns, get in touch with us today.
For SNFs and independent nurses, our advanced education opportunities and professional partnerships offer the level up you need. With expert-led instruction and hands-on training, you can reduce hospital readmissions, improve patient experience, and lower facility costs. Our programs invite you to build the confidence and competence necessary for effective wound care.
